
Demolition of Mary Hitchcock Memorial Hospital in Hanover. Courtesy photo.
As workers dug through the imploded rubble of the original Mary Hitchcock Memorial Hospital in Hanover in the mid-90s, they unearthed a promise buried beneath its foundation nearly 102 years before.
“It is a memorial of one of the noblest and best of God’s gifts to the human race,” read a love letter left in a time capsule buried beneath the building at the time of its construction by Hiram Hitchcock for his childhood sweetheart and wife, Mary, for whom he’d named the hospital.
“God grant that this hospital may be all, and more than all that she would have it to be. She was my life here. May God in His infinite mercy unite us again.”
In the 125 years since Hiram penned those words, Mary Hitchcock Memorial Hospital has grown into the influential powerhouse that is Dartmouth-Hitchcock Medical Center and Dartmouth-Hitchcock Health system.
But just as any good love story, Dartmouth-Hitchcock, based in Lebanon, has experienced its share of triumphs and challenges over the years. The place that played host to the first diagnostic X-ray is the same place that came under fire in recent years for understaffing NH Hospital in the midst of a mental health-care crisis. The place that was among the first in the country to organize a group medical practice and form affiliations is the same place that came under government scrutiny over antitrust concerns. The place that was an early adopter of air ambulances, built the world-renowned Norris Cotton Cancer Center, and developed the skills of thousands of promising doctors in the halls of its affiliated medical school is the same place making news for contract disputes with doctors, mass layoffs and a period of financial instability.
And yet, Dartmouth-Hitchcock’s highs are more impactful than its lows. Its most recent rise has come under the new leadership of Joanne Conroy, MD, president and CEO of Dartmouth-Hitchcock Health. Most recently the CEO of Lahey Hospital and Medical Center in Burlington, Mass., Conroy took the helm of a listing ship in June 2017 and has set a course for righting it.
The Hitchcocks’ Legacy
Hiram Hitchcock and Mary Maynard grew up together in Drewsville, NH, and married in 1858.
Hiram, a successful hotelier in New Orleans, moved his bride to New York and with two business partners built the Fifth Avenue Hotel in Manhattan. The move made Mary an instant hostess to luminaries such as Presidents Grover Cleveland and Theodore Roosevelt.
But the Hitchcocks were not immune from tragedy and hardship. The couple’s daughter died when she was a month old. Their son, born a year later, died at 14 months. Three years later at age 34, Hiram, himself in poor health, decided to retire.
In 1879, Hiram once again ran the Fifth Avenue Hotel. He also went on to help found Madison Square Garden and served as its president. Over the next several years, Hiram and Mary split their time between homes in Hanover and New York. But in 1887, Mary died of “unknown causes” at the age of 53.

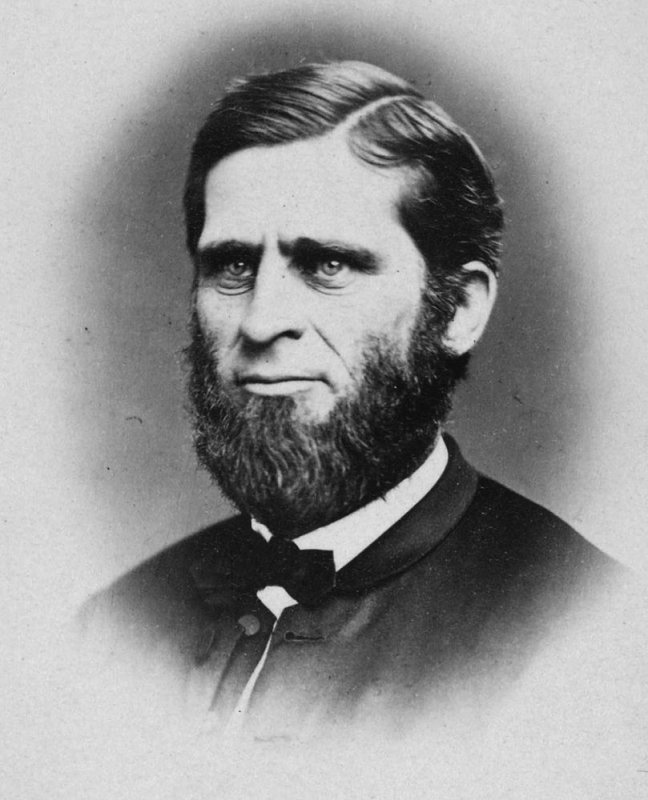
Mary and Hiram Hitchcock. Courtesy photos.
Two years after her death, Hiram funded construction of Mary Hitchcock Memorial Hospital in Hanover. In all, the facility cost an estimated $200,000 and came complete with massive structural pillars, a carved Sienna marble fireplace, and a mosaic tiled floor. The hospital opened May 3, 1893, to serve the Upper Valley’s residents and acted as a teaching hospital for Dartmouth Medical School students and a nurse training center.

The original Mary Hitchcock Memorial Hospital. Courtesy photo.

Nursing students at the hospital. Courtesy photo.
The Evolution
Dartmouth Medical School was founded by Nathan Smith in 1797 to address the lack of trained physicians in the region and was only the fourth such school to open in the United States.
Nearly 100 years later, the school and hospital became inextricably linked when the dean reached out to his friend Hiram to fund the hospital. And innovation has followed ever since.
In 1927 four doctors—using a model they’d experienced while training at the Mayo Clinic—formed the Hitchcock Clinic, a multispecialty partnership that was among the first organized group practices in the U.S. The group eventually won the approval of the Mary Hitchcock Memorial Hospital board to practice in the hospital. “They focused on Mary Hitchcock [Memorial] Hospital; that was the bulk of their practice,” says Jim Varnum, who served as president of the hospital for 28 until he retired in 2006. “But they also began to develop outreach clinics in various communities.”
By the 1940s, the hospital introduced a flying ambulance service and had become a corporation—Dartmouth-Hitchcock Inc.—although in 1983 it would become a nonprofit. The hospital and school continued to innovate and by 1972 was ready to open Norris Cotton Cancer Center, which today is one of only 45 comprehensive cancer centers in the nation.

Dartmouth-Hitchcock Inc.’s flying ambulance service, circa 1950. Courtesy photo.

The Dartmouth-Hitchcock Advanced Response Team team provides ground and air medical transportation services to the medical communities of Northern New England. Courtesy photo.
In 1991 the hospital was outgrowing its space and officials were looking to further establish it as the state’s only academic medical center, so they moved to Lebanon. Varnum, who led the hospital during this transition, says they initially wanted to stay in Hanover. However, the Hanover Planning Board told hospital officials that if they were allowed to expand this time, they would not be approved for future expansions, nor would the medical school. That did not jive with the vision hospital and school officials held, so they picked up stakes.
When it was completed, Dartmouth-Hitchcock Medical Center boasted a new approach to design, with myriad skylights to let in natural light and large airy corridors. With the new campus up and running, the main Mary Hitchcock Memorial Hospital building in Hanover was demolished in 1995.
Changing the Landscape
For more than two decades, the hospital has continued to grow and expand its reach across the border into Vermont and around the state. Today, Dartmouth-Hitchcock Health (D-H Health), as it has been known since 2009, provides access to more than 1,000 primary care doctors and specialists, and includes the Norris Cotton Cancer Center, the Children’s Hospital at Dartmouth-Hitchcock (CHaD), four affiliate hospitals, and 24 ambulatory clinics across NH and Vermont. These clinics include a 150,000-square-foot center in Nashua and a 120,000-square-foot building in Manchester that houses primary and specialty care services, a lab, radiology services, and an ambulatory surgery center. D-H Health also owns and operates Visiting Nurse and Hospice for Vermont and NH.

The Children’s Hospital at Dartmouth (CHaD). Courtesy photo.
Moreover, the Dartmouth-Hitchcock system trains nearly 400 residents and fellows annually, and performs research in partnership with the Geisel School of Medicine at Dartmouth College and White River Junction VA Medical Center in White River Junction, Vt.
“As health care has changed dramatically over the years, [Dartmouth-Hitchcock] has really been on the forefront of the health care delivery system,” says Steve Ahnen, president of NH Hospital Association in Concord, citing its affiliation strategies and work with other hospitals to provide telehealth services.

Dartmouth-Hitchcock partners with health care providers and facilities throughout northern New England to provide telehealth care to patients. Courtesy photo.
Its affiliation efforts, however, have hit speed bumps. In 2010 the Medical Center tried to affiliate with the second largest hospital in the state, Catholic Medical Center in Manchester. In addition to pro-choice advocates worrying the affiliation would lead to curtailing abortion and birth control services because of CMC’s Catholic core, other officials were concerned that two large medical centers joining forces would create a medical monopoly. In the end, the NH Attorney General put the kibosh on the affiliation.
Dartmouth-Hitchcock also tried twice in the past few years to affiliate with NH’s second largest health system, Elliot Health System. In 2017, both parties walked away from the deal but agreed to find ways to unofficially work together.
That said, Dartmouth-Hitchcock Medical Center continued to form strategic partnerships with other hospitals, including Alice Peck Day in Lebanon, Cheshire Medical Center in Keene, and New London Hospital, as well as Mount Ascutney Hospital and Health Center in Windsor, Vt.
While Dartmouth-Hitchcock didn’t invent the strategic partnership, it did seem to spark the trend in NH’s health care sector and has used it more often than others to broaden its reach.
One criticism of this move toward affiliated hospital systems, particularly Dartmouth’s, has been the notion that community hospitals that affiliate with Dartmouth in short order simply become satellites of the larger Lebanon mothership. For some hospitals, critics argue, this translates to a reduction in some services: for example, the shutdown of the birthing center at Alice Peck Day. Another result can be patients having to drive to Lebanon to access services they used to get down the street.
But Conroy strongly disagrees with that critique. “The big challenge is figuring out what services to deliver where, and we actually do that with our hospitals; we don’t do that to our member hospitals,” she says of including hospital members in decision-making.

Joanne Conroy, president and CEO. Courtesy photo.
Conroy says Alice Peck Day officials came to Dartmouth-Hitchcock and asked them to consider taking on their birthing patients. “They had a very difficult time retaining the staff they felt they needed for the unit,” she says. “Frankly, the obstetrician just said, ‘We’re not doing enough volume to maintain the expertise.’ They were down to almost 150 [births annually].
That’s like a birth every three days, but it’s a 24/7 operation. That’s why we merged the units.
We did not get rid of [birthing services at] Alice Peck Day, we just said we will have a combined unit here.”
There were also concerns when Cheshire Medical Center, Dartmouth-Hitchcock closed its inpatient mental health unit. Conroy says, “They were probably the last to close their [inpatient] mental health unit. A lot of people actually did.” She says the closure was the result of an inability to recruit physicians to the area.
She says D-H Health invested significantly in improving the hospital’s ICU to allow more patients to have procedures there. “We are starting to really encourage hospitals that are closer to Cheshire Medical Center to send patients there,” she says. “We are actually seeing more and more people actually drive south rather than north because there are so many things they can actually get at Cheshire Medical Center.”
Dartmouth-Hitchcock also spearheaded the New England Alliance for Health, an affiliation of 18 critical access and community hospitals in NH, Vermont and Massachusetts that coordinate care and resource planning. “We work together to create a stable financial network of care,” Conroy says. “The majority of the members we have added have actually been critical access hospitals. They are hospitals that probably wouldn’t exist if we hadn’t come together to make them stronger.” Through the Alliance, those small hospitals can access more significant discounts on products than they could on their own, including pharmaceuticals, she says.
Challenges Abound
Two years ago, though, the state’s largest health system hit a rough patch. A restructuring plan, aimed at moving Geisel’s psychiatry department to Dartmouth-Hitchcock to address an anticipated $30 million shortfall for the school, ended up causing a slew of new problems.
Geisel had long held the contract for care at NH Hospital, the state-run, taxpayer-funded mental health facility in Concord, which was up for renewal in 2016. With the restructuring in full swing, Dartmouth-Hitchcock submitted a bid for the contract and turned out to be the only bidder.
However, many of the psychiatrists at NH Hospital balked at the new terms of the contact, causing Dartmouth-Hitchcock to rescind its offer. Several NH Hospital staffers left, formed a practice group and tried to apply for the contract themselves, though were unsuccessful as it was past the state’s deadline. By September 2016, the state agreed to award the contract to Dartmouth-Hitchcock with the assurance that NH Hospital would be fully staffed. Shortly after the contract was awarded, Dartmouth-Hitchcock announced it was laying off 84 staffers due to a $39 million operational deficit. Based on this news, a bond rating agency downgraded Dartmouth-Hitchcock and another put it on a credit watch list.
Rounding out the year, former Norris Cotton Cancer Center director Mark Israel sued Dartmouth-Hitchcock, claiming he’d been wrongfully fired after raising concerns over potential misappropriation of funds raised by The Prouty, a large, profitable annual fundraising race that benefits cancer research and patient support services. Though Israel’s case was ultimately dismissed and it was determined Dartmouth-Hitchcock did not do anything illegal, the hospital did pay back money that went for operational costs but not research or support services.
By May 2017, Gov. Chris Sununu said Dartmouth-Hitchcock was keeping NH Hospital understaffed and not living up to its contract. He argued that the CEO of NH Hospital, Robert McLeod, needed to go, which he did. Dartmouth-Hitchcock CEO James Weinstein also ended his nearly six-year tenure in early 2017 with the announcement that he was retiring that summer.
“When I arrived in Lebanon a year ago to become the CEO of Dartmouth-Hitchcock, I took the helm of an organization that endured tremendous challenges over the previous 18 months,” Conroy says of her June 2017 appointment to head the hospital. “As you know, in 2016 Dartmouth-Hitchcock underwent a significant financial crisis, resulting in a reduction in workforce. Employee morale was low.”
The first thing she did was get the senior leadership team and board of trustees together to evaluate everything: the health system’s leadership structure, core business strengths, workforce needs, clinical and administrative operations, and measurement systems. “All this was done with the focused goal of returning Dartmouth-Hitchcock to its previous performance as a highly functioning organization,” she says.
Conroy, along with the leadership team, identified priority areas and used those as the basis for a Performance Improvement Plan, or PIP. The PIP focused, Conroy says, on operational and financial stability, employee engagement, quality and safety, and strategy development and execution.
“The PIP that we put into place has made major strides in reaching all the goals of these priorities,” she says. “Our financial picture has brightened across a number of fronts, and we now show a significant increase in operating margin over last year—one of the major indicators of our financial health.”
She also says the hospital has taken a number of steps to improve employee engagement based on “the simple act of listening to our staff,” including conducting a number of employee focus groups and surveys to get a sense of employees’ thoughts, feelings, ideas and concerns.
“We’ve identified a number of issues that we’re taking on, including staffing levels, compensation and benefits, and clarity about Dartmouth-Hitchcock’s mission, vision and values,” she says.
Further, Conroy says they are continuing to push for “greater quality and safety standardization, as well as monitoring and measuring care outcomes and patient experience.”
She says in this regard some areas of the organization have seen “stunning improvements” in preventing serious safety issues, including outcomes that are “far better than national benchmarks.”
“And we are now deep into a system-wide strategic planning process that will guide the future,” she says. “I’m confident we’ll come out of this strategic planning process later this year with a clear road map that will lead D-H into the future and ensure our ability to continue to provide the best care to our patients and the communities we serve.”
On the Horizon
So far, things do seem to be looking up. On the news of the improvement of Dartmouth-Hitchcock’s financials, the two major credit agencies—FitchRatings and Standard & Poor’s—affirmed their “A” ratings for the hospital system and upgraded the outlook to “positive” from Fitch and “stable” from S&P.
Fitch stated that the rating and outlook “reflect Fitch’s expectation that Dartmouth-Hitchcock Health will continue to improve upon the results of its Performance Improvement Plan [and] … continue to demonstrate strong cost management.” S&P stated that Dartmouth-Hitchcock anticipates it will issue up to $700 million in bonds to refinance the majority of its system-wide debt and acquire new money for capital projects.
Following this bright financial news, in the June issue of Modern Healthcare Magazine, Conroy was named one of the 50 “Most Influential Physician Executives and Leaders” for ensuring the “$58 million turnaround in the health system’s finances,” the upgraded bond ratings and her work on improving engagement and retention among staff.
Conroy also says things seem to have stabilized when it comes to the NH Hospital contract.
She says Dartmouth-Hitchcock has resolved the staffing dispute and believes the state is satisfied that they are at the appropriate staffing levels. She also praised the work of the new CEO of NH Hospital, Lori Shibinette, who has suggested that the state doesn’t necessarily need more inpatient beds, but rather more facilities for outpatient care and recovery after release from NH Hospital.
While there are no plans to expand the number of psychiatric beds at Dartmouth-Hitchcock either, the hospital is renovating rooms that house mentally ill patients to meet new regulations. “Any physical plant that could present a physical risk for a patient that could be suicidal has to be eliminated,” she says, “and that means all your bathrooms have to be redone; there can’t be any wires—there is a whole art to creating a ligature-free environment.
Also, patients need to be monitored constantly now. Every 30 minutes is no longer acceptable.” The project began in January and will cost millions to complete.
Further, she says, Dartmouth-Hitchcock is offering psychiatric telehealth services in an attempt to share its psychiatric resources with patients and facilities across the state.
TelePsychiatry offers access to board-certified psychiatrists who provide 24-hour per-day psychiatric consultations.
With the help of a $2.7 million, two-year federal grant, Dartmouth-Hitchcock expanded resources for The Moms in Recovery program, which offers screening and treatment for pregnant women at seven maternity care practices around the state in developing their own medication-assisted treatment programs.
Looking ahead, Conroy says Dartmouth-Hitchcock is working on making improvements to benefits and investments in wage scales, professional education and merit programs to help attract and retain talent.
Regionally, she says, Dartmouth-Hitchcock is preparing for facility expansions in Concord, Bedford and Manchester to grow their primary care practices and access to specialists in the southern part of the state.

Doctors performing surgery at Dartmouth-Hitchcock Medical Center. Courtesy photo.
Conroy says they are also evaluating options to relieve capacity issues in Lebanon, including redirecting lower-acuity patients to member facilities based on where the patient lives and their medical needs.
As for future partnerships, Conroy says they have been in talks with organizations across New England. “As I look ahead, I’m optimistic about D-H’s future,” Conroy says. “We are aligned with our goals, increasingly engaged and fully committed to continuing to provide the best care for our patients across the region.”
