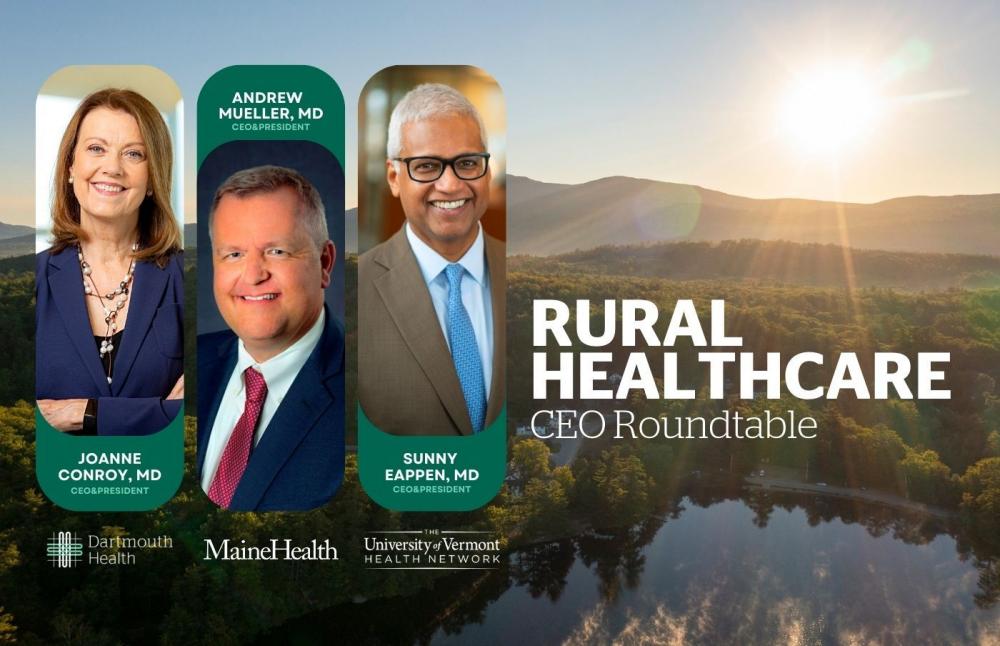
CEOs from health systems in NH, Maine and Vermont recnelty came together during e CEO roundtable to discuss the growing challenges hospitals face in the rural Northeast. Dartmouth Health CEO and President Joanne M. Conroy, MD, joined MaineHealth CEO Andrew Mueller, MD, and The University of Vermont Health Network (UVMHN) President and CEO Sunny Eappen, MD, MBA in a roundtable discussion about the crisis in rural healthcare on May 22.
The roundtable was live-streamed on YouTube from Dartmouth Health’s Dartmouth Hitchcock Medical Center. The recording can be viewed at go.d-h.org/ceo-roundtable.
“Seventy percent of hospitals nationwide were in the red in 2022, so we're not alone. In rural America, the challenges are more difficult to navigate, especially in New England where our systems are located, and which has not bounced back like other areas of the country post-COVID,” said Conroy. “Although the [federal] provider relief funds were crucial and allowed our hospitals and rural hospitals to recover, post-recovery we are facing a host of challenges all at once, led by a persistent healthcare workforce shortage, which affects each of our institutions.”
Conroy said labor costs continue to escalate primarily because organizations must pay premiums either for their own employees to work overtime to cover gaps, or they must pay contract labor – commonly referred to as ‘travelers’ – often more than three times the rate that their own employees are paid. A reality that can contribute to employee discontent and attrition.
The leaders of the largest healthcare systems in northern New England and the North Country of New York discussed what it means to be an academic health system, the workforce challenges, including recruitment, housing and childcare, as well as payer, regulatory and inflation challenges, and innovations that preserve and improve access to high-quality care.
“Discussing our common challenges as rural health systems is so important, and by working together I am certain that we can preserve and improve access to high-quality care for patients in our region,” said Sunny Eappen, MD, MBA, President and CEO of the UVM Health Network. “I do see a bright light in the face of this turmoil: We have an opportunity now to make truly positive lasting change while we chart a path forward. That means getting creative with the way we deploy our talented workforces, allowing our physicians, nurses, and all of our staff to work at their highest level; advancing telehealth in new, efficient and exciting ways that make scheduling appointments and getting answers easier for patients and providers; and leading the way as diverse, equitable and vibrant organizations. Of course to do all this, we will need the support of our federal and state governments, and we will need commercial payers to reimburse us at levels that allow us to continue providing care to their members, who are our patients.”
As academic medical centers, Dartmouth Hitchcock Medical Center, Maine Medical Center and University of Vermont Medical Center are crucial ‘safety nets’ for New Hampshire, Maine and Vermont. While smaller critical access hospitals may close beds due to staffing challenges, the academic medical centers must keep beds open for the sickest and neediest patients that cannot be cared for in smaller facilities. The leaders agreed that labor costs have increased 12-15 percent post-pandemic, and these are costs that they are unable to pass along to consumers or insurance companies, which has created significant financial gaps for their systems.
“We're our state's largest private employers. And we have a big economic impact in terms of the ability to create jobs, to give people good pay, and to really help stimulate the economies of the states we serve,” said Andrew Mueller, MD, Chief Executive Officer, MaineHealth. “If we are impacted to the point that we have to reduce services, not only do we run the risk of individuals being harmed by failure to access care, we also run the risk of really damaging some of our rural communities economically and socially.”

 Current Issue - July 2024
Current Issue - July 2024