-62-sm.jpg)
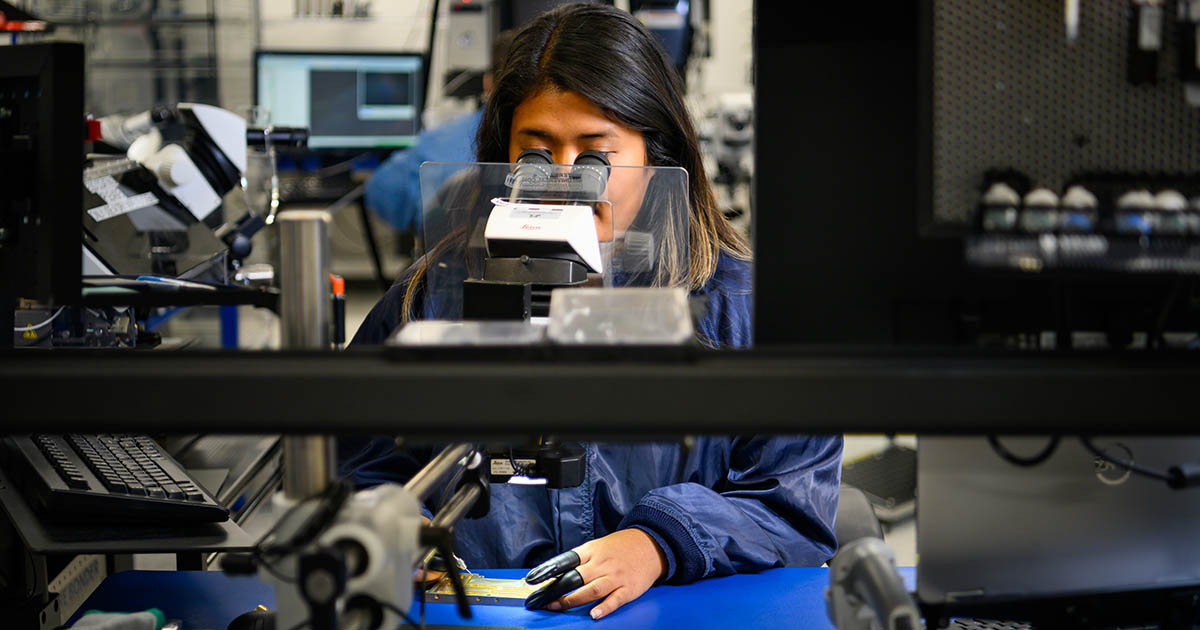
Home Care Nurse, Erica Seawards of Cornerstone VNA, with a patient (Photo by Keith Allen Chick)
Amy Moore has strong feelings about the value of home care for patients of all ages because she’s seen what can happen when care isn’t available. She is vice president of external relations at Ascentria Care Alliance and president of the Home Care Hospice and Palliative Care Alliance of NH. Ascentria is one of the largest providers of non-medical home care in NH, providing services to over 360 clients with 300 caregivers. But 17 years ago, she was a case worker helping a roofer in his late 20s who took a bad fall.
“In order to stay home independently, he needed help,” she recalls. “He’d been with us for years, and we all became friends.” Moore moved into other positions at Ascentria over the years, and three years ago got a call about that patient. He had moved to another agency because Ascentria couldn’t find a caretaker for him, then that agency had to turn him down as well. “His case manager knew that we were all close with him, so she called to let us know what happened. He was trying to transfer from his wheelchair to his bed and he fell, hit his head and died,” she says.
She tells the story not to be an alarmist, but to share a hard but often invisible truth. In-home care services are a matter of life and death, and they are teetering on the brink. Prior to COVID, the percentage of family, friends or loved ones providing home health care through a Medicaid program was about 40%; now it’s 85%. The rest is provided by home health care companies like Moore’s. Home health care organizations that provide care face challenges with staffing and a looming federal cut in reimbursement rates. For families, care might be available but is often unaffordable, Moore says.
“That tells you our system is broken,” says Moore of the many family members and friends providing care. “Because those aren’t all people who want to do it. I can tell you there are people that up and moved across the country or left their career because they couldn’t find anyone to care for their loved one, and eventually they had to step in. It’s a beautiful thing when it works. But it being at that number, at 85%, that tells you we have an issue.”
Moore worries that her aging mother, still in good health for now, might need such services someday. “Every time I see her, I say, and this is what I tell everybody I know, ‘Don’t think that if something happens you can pick up the phone and call and get help because chances are you can’t, and it’s just going to get worse.’”
From Fearful to Hopeful and Back
Reimbursement rates have always been a big challenge for home health, which are mostly government funded and serviced by nonprofit organizations. The future of home health care in NH was more promising in 2023, when Ascentria received a 42% Medicaid rate increase. Medicaid service rates were also increased for a variety of services, including home health and personal care aids. The state budget that took effect that year also had a 3% increase in reimbursement rates for providers.
Now, in addition to billions in reduced Medicaid spending, the home care industry is concerned about a possible reduction in Medicare reimbursement. The Centers for Medicare & Medicaid Services has proposed a 6.4% reduction in Medicare payments to home health agencies for calendar year 2026, an estimated $1.13 billion decrease.
Back in 2023, Ascentria and Waypoint warned that without higher payments, they’d have to end home care services, leaving clients waiting for a nursing home bed, seeking help from family, or being left on their own.
“We were at the point where we were seeing people go without care, and were seeing what was happening and the devastation, and frankly, we were going to have to close our programs if investments weren’t made in this space. Luckily, at that time, the state stepped up,” says Moore.
Thanks to those state increases, NH’s largest home care providers have not taken steps to dramatically curb services like Andwell Health Partners in Maine which late last year announced it would scale back its coverage area in Maine and significantly reduce in-home skilled pediatric services.
Andwell is not alone. The number of home health agencies in the country has been decreasing since the peak in 2013 when there were 12,613 active agencies, according to Statista.com. As of 2023, the number of agencies has dropped to 11,506.
Those that remain struggle to maintain the needed levels of service, with an aging population creating greater demand. Existing workforce challenges are made more difficult by aggressive immigration enforcement, impending federal cuts to Medicaid, and a strapped state budget.
“In New Hampshire, we continue to have home health agencies available to serve our population across the state,” says Keliane Totten, CEO of the Home Care, Hospice and Palliative Care Alliance of NH. “But it’s important to note from a national perspective in the U.S., since 2020, half of all of counties have lost some home health care. Some agencies are challenged to provide timely care and also have workforce challenges.”
Catherine Frasco, vice president of Home and Community Services at Elliot VNA in Manchester, underscores the strain proposed reimbursement cuts place on agencies. The final changes in reimbursement will be finalized in early November. “It’s the biggest cut in history and comes at a time when half the counties in the U.S. have lost home health agencies,” she says of the Centers for Medicare and Medicaid Services proposed reductions, echoing Totten. “Should those reductions go into effect it will make access to home healthcare even more difficult. These are devastating cuts.”
Frasco notes that home health is not only more affordable than hospital care by keeping patients out of facilities where they risk infection and isolation but also aligns with what most people want: to age in place. “The reimbursement is probably our biggest challenge,” Frasco says.
An Array of Services
Home health care ranges from an aide who visits a few hours each day to help with activities of daily living, offering companionship and performing some basic medical tasks, to a private duty nurse who provides skilled nursing care to patients in their homes.
In-home providers often see firsthand the challenges patients face, such as food insecurity, medication mismanagement, lack of caregiver support, or even physical hazards in the home, Frasco says. “When you truly have your eyes on those barriers, then you can truly make a difference in a care journey toward improving outcomes,” she says.
On the clinical side, Frasco says patients are being discharged with more sever medical conditions, or higher acuity, than ever before. This could include triple bypass patients, advanced wound care, infusion therapies, and joint replacements, all requiring complex in-home services. “Consequently, in-home care has had to adapt, elevate, and be able to treat higher acuity patients in the home,” she says. That is why Elliot VNA deploys a large interdisciplinary team including nurses, physical and occupational therapists, social workers, and LNAs to wrap their arms comprehensively around patients and their families.
But staffing those positions is a challenge, Frasco says. “We can’t fill that workforce fast enough,” she says, noting the reliance on virtual visits and remote monitoring as partial solutions. Elliot VNA has a virtual visit nurse supporting field staff, while patients track daily vitals through connected devices. “That supports both patient care and the workforce challenge.”
Others are adapting as well. As the reimbursement landscape shifts, Cornerstone VNA in Rochester, a nonprofit visiting nurse provider serving more than 45 communities in NH and Maine, is using technology to fill in gaps, including using telehealth and chronic care management tools, and exploring artificial intelligence to streamline daily tasks.
Yet growing demand makes it challenging to meet the needs in the community. “Back in 2001, a nurse might see a patient two or three times a week for eight or nine weeks,” says Jennifer Ufkin, president and CEO of Cornerstone VNA. “We can’t do that anymore. Now, we do more visits upfront and taper down. Families and patients are carrying more responsibility. We’re trying to supplement that through virtual services, education, and caregiver support.”
One of the most popular programs in NH is the Medicaid-funded Choices for Independence, which helps eligible adults remain in their homes and communities rather than moving into a nursing home. As part of this program, qualified family members or friends can be trained and paid to offer in-home care services.
Home health care providers were nervous about the future of home care services when NH House budget writers earlier this year proposed a 3% cut to Medicaid providers. Then it was reversed in negotiations with the Senate and Gov. Kelly Ayotte.
“We are extremely grateful that the reduction did not stick and we didn’t experience a cut, but the truth of the matter is at this point in our state, without having an increase, the status quo is essentially a cut,” says Totten, noting her industry is competing for the same workers who might otherwise work in hospitality at higher rates or be recruited by agencies in bordering Maine or Massachusetts that pay more.
Totten says providing care at home, when it can be provided, is better for the patient and more cost-effective for the payer, whether that’s the patient, a private insurer, or the government through Medicaid or Medicare. “We need to continue to advocate for adequate reimbursement for these much-needed services,” says Totten.

Physical Therapist Dan Wightman of The Elliot VNA with a patient, Michael. (Courtesy of The Elliot VNA)
Balancing Costs and Needs
The proposed 6.4% reduction in Medicare payments beginning in 2026 has many providers worried. “That proposed rule is a significant reduction in payment for our skilled care,” says Totten. “That would absolutely have ramifications. We would see agencies need to shrink service areas.”
Beth Slepian, president and CEO at Granite VNA, a nonprofit providing health and wellness services, including home care, hospice and palliative care, pediatric and maternal child services, says one of the greatest challenges in the current environment is managing consumer expectations. “People may have the expectation they’re going to get checkups two times a week but may only need it once,” she says, explaining that national standards drive how care is delivered.
But quality has a cost, and some of the existing financial models no longer align with how care is delivered. “Medicare Advantage doesn’t cover the cost of services we provide, and many of those plans require authorization,” Slepian says. “We’re taking care of people, and our clinical teams are resilient—they adapt to provide the best care available. But we need to be able to pay our bills.”
Another complication is that patients have more medically complex issues than in the past, requiring services that previously would have been delivered in hospitals or long-term care settings, says Julie Stone, vice president of strategy at Granite VNA. “Our caregivers need to be educated and prepared to handle this level of care, and we have to be nimble in how we deliver that,” Stone says. “We’re a nonprofit, so we’re doing a lot of mission-driven programs with no compensation like wellness classes, prevention, and foot care, all designed to help patients avoid hospitalizations and remain at home longer.”
Some providers paint a starker picture. Ufkin of Cornerstone VNA says the state’s home health and hospice sector is at a breaking point. “It’s been a chaotic and frustrating situation,” Ufkin says. “In just five years, our home health census has grown by 43%, and on the hospice side we’ve seen an 8% increase. As one of the two oldest states in the country, we’re finally seeing the baby boomer need in a significant way. The challenge is staffing to meet that demand.”
Recruitment, she notes, remains one of the organization’s greatest hurdles. “We’re competing against hospitals and nursing facilities for the same workforce. If we don’t have the staff, and then we face reductions in Medicare and Medicaid funding, agencies like ours simply can’t meet the need.”
At the state level, funding is flat while costs continue to climb. “For every dollar Medicaid pays, it costs us $2.08 to care for a patient,” Ufkin explains. “That math doesn’t work. It’s very hard for agencies to provide care with Medicaid changes, and Medicare cuts on top of that mean something has to give. We need some margin to care for our most vulnerable.”
Medicare Advantage plans, which many seniors now rely on, add another layer of strain. “Those plans often pay per visit,” she says. “We’re lucky if direct costs are covered, never mind overhead. If these changes continue, agencies will go under. We need something to supplement and stabilize the system.”
That’s why Ufkin recently traveled to Washington, D.C., advocating for the Home Health Stabilization Act of 2025. The bipartisan bill, H.R. 5142, would delay further Medicare payment reductions for two years, giving the Centers for Medicare and Medicaid Services time to reassess reimbursement models.
“Home health is not overpaid—we account for less than 5% of total healthcare spending,” Ufkin says. “We need a better system at the federal level to rein in Medicare Advantage and make sure patients get the care they need. Passing this bill is the first step.”
Home health is also complicated, and not as cheap as it is sometimes made out to be. Stone pushes back against a long-standing myth that home-based care is always cheaper to deliver. “It’s always perplexed me,” she says. “It’s not necessarily less expensive when you’re dealing with medically complex patients in their homes.” She adds that a ‘home’ “might be a cul-de-sac in a suburb or it might be a rural camper without running water. “But we’re committed to serving all members of our community,” she says.
Despite challenges, Granite VNA focuses on continuous innovation and efficiency. “We’ve looked hard at our processes, from back office to how clinicians deliver care, and we’ve made changes,” says Slepian. “This isn’t work for the faint of heart.”
It’s two steps forward, three steps back, as far as Moore, president of Ascentria Care, is concerned. “We’re basically slowly navigating our way back to the way things were in the 40s and 50s, when these services didn’t exist. It was up to the family. It’s a big reversal in that regard,” she says.
So far, services have not been lost in NH, but they are harder to secure. “There absolutely are agencies that in the past were able to send staff the next day, but that wait has become longer and more and more challenging,” Totten says.
-35-sm.jpg)
Cornerstone VNA Continues a History of Community Care
Modern nursing as we know it traces its roots to Florence Nightingale, the English social reformer who transformed health care during the mid-19th century. Nightingale emphasized sanitary practices, compassionate care, and professional training—principles that redefined nursing as both a science and an art.
Her vision carried into the 20th century, when community-based organizations began providing medical care outside the walls of hospitals. In 1913, one such organization took shape in southeastern NH: Cornerstone Visiting Nurse Association (VNA) in Rochester. Founded when home visits by nurses were still a novel concept, Cornerstone VNA has grown into one of the state’s largest nonprofit providers of home health, hospice, private duty, and community services.
Over more than a century, Cornerstone VNA has evolved alongside the profession itself. Nurses today function as caregivers, educators, and advocates for patients, serving on the front lines of an increasingly complex health care system. Their responsibilities extend far beyond bedside care. They administer medications, operate advanced medical equipment, and provide critical guidance to families navigating illness and recovery.
For Jennifer Ufkin, Cornerstone VNA’s president and CEO, that combination of technical skill and human connection defines why the organization remains vital.
“Despite mergers and acquisitions across the industry, we’re still strong because of our culture and mission,” Ufkin says. “That’s what keeps me here. We’re investing in free educational series, caregiver cafés, and volunteer programs to support families. Day after day, what grounds me is how grateful people are for our services.”
But sustaining that mission, she cautions, will require more than dedication at the local level. As federal reimbursement rates fall and policy changes threaten community-based care, organizations like Cornerstone VNA are forced to do more with less.
“We’re facing growing needs with fewer resources,” Ufkin says. “It’s going to be very hard to manage the baby boomer generation—and the generations after them—if the cuts keep happening.”